Antibiotics would not be available in the pharmacy for another 25 years when surgeon Rickman Godlee delivered a Friday Evening Discourse at the Royal Institution entitled "Back to Lister", in 1915. The lecture was based on the book he was writing on the life and work of his uncle Joseph Lister, pioneer of antiseptic surgery.
So, what did science offer the wounded soldier in World War I? Medicine almost seemed to be going backwards. But it turned out that a simple dose of salts could work wonders.
Spray away
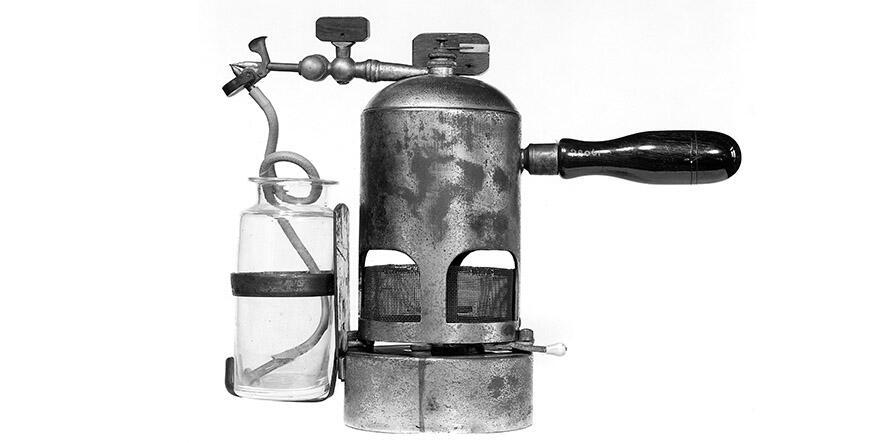
Antiseptics, which we tend to think of today as a momentous surgical advance, had proved to be a mixed blessing. After Lister introduced them, the effect of powerful agents like carbolic acid (phenol) on surgeons’ ungloved hands intimated their damaging effects on exposed tissue.
It comes as a surprise, Godlee said that Lister "more and more diminished the strength of and the amount of his antiseptics."
And of antiseptic aerosols: "Lister at last came to the conclusion that the spray was unnecessary…"
Rather than bacterial attacks from the surrounding air, said Godlee:
Land and water attacks were far more dangerous. The germs on the skin of the patient, the dirt on the hands of the surgeon, the unpurified sponge, the dried clot on a badly cleaned instrument – these were the dreadnoughts and submarines, the howitzers and hand-grenades; these were the sappers and miners that really decided the fate of the campaign. Thus it became obvious that the precautions taken against such sources of danger, which, though they were adopted from the first, had been overshadowed by the attention devoted to the air-raids.
Quoting another military surgeon, Godlee continued, "In this trench warfare you must remember that, if a man is hit, he often falls into filthy mud and water… and the water is hopelessly polluted, and soaks his clothes and his wound."
Godlee summed up: "Antiseptics are being very largely used though with most disappointing results." However, "Undiluted carbolic acid is, according to our present lights, the antiseptic most likely to be practically useful in the rough-and-tumble practice of the battlefield."
Rough and tumble? At least the medics had an understatement ready to make you feel better.
Often, the first people to apply antiseptics to the wounded were untrained comrades. They splashed it on, and burnt the exposed tissue. Medical researcher Almroth Wright investigated, though an audience at the Ri would only hear his findings after war had been raging for another two years.
Click and collect
Meanwhile, James Mackenzie Davidson, a radiologist who consulted at military hospitals, was also trying to do what he could for wounded soldiers and came to the Ri to deliver a Discourse on "Electrical Methods in Surgical Advances" in 1916. The potential of X-rays was recognized from the moment of their discovery in 1895, but they usually only depicted a view of the body in two dimensions, a limitation which would remain for another 50+ years.
"Having ascertained the position of the bullet in the body we have at hand, fortunately, other electrical aids for the surgeon when he comes to deal with the problem of its extraction. One of the most useful of these adjuncts is the telephone probe… It consists of a telephone to one terminal of which may be attached the surgeon’s steel, silver or nickel-plated instrument, while a carbon plate is attached to the other terminal which is applied to the patient’s skin, moistened… When any of the instruments come into contact with embedded metals, such as lead, nickel, copper, iron, or the iron alloys used in shell manufacture, a loud click is elicited…"
Alternatively, "a large electromagnet is excited by an alternating current and held over the suspected part. If the magnetic field which is thus created embraces the embedded projectile, a vibratory motion is induced in the projectile… The surgeon palpates the part, and becomes instantly aware of any vibration of the tissues."
Dressing to kill
Almroth Wright was a pathologist and immunologist, one of a new generation able to find a career in the medical laboratory. He spent the latter half of his life at St Mary’s Hospital Paddington where Alexander Fleming arrived a few years later, as his newly qualified assistant.
In a long lecture in 1917, Wright discussed the healing, infection and dressing of wounds, including the normally mildly antibacterial action of blood serum. This led up to laboratory experiments with Fleming’s ‘artificial war wound’, a curious piece of glassware, made with deep pits or ‘diverticula’ representative of real bullet and shrapnel wounds.

"To imitate the conditions obtaining in the actual war wound we fill both the tube and its diverticula with an infected trypsinised serum." By the latter, he meant degraded serum as typically found in wounds.
"We now empty the tube, leaving behind of necessity in the diverticula a certain amount of the original infected fluid. We then fill with an antiseptic; and the future of the infection will now depend on the penetrating power of the antiseptic. If the antiseptic penetrates into the infected fluid sterilisation will be obtained; if it fails to penetrate microbes will survive. To test our result we empty out the antiseptic, refill with trypsinised serum, and incubate."

His discourse finally resolved in quite the opposite direction to Godlee. Wright’s studies indicated that healing was helped by the easy migration of white blood cells into a wound to fight infection, which was inhibited if the wound dried up, or was burnt by antiseptics, and might kill the patient.
"The first thought of every man would probably be that the wound should be most carefully disinfected at the outset. But what happens in burns shows that to start in open wounds with a sterile surface avails nothing. A burn is at the outset absolutely sterile, and quite notoriously… it tends to become very rapidly septic… It is just the same with war wounds. These become heavily infected even when they are drenched at the outset with undiluted carbolic acid."
A 5% salt solution was his advice to clean the wound, and keep it dressed and wet.
Soldiers could still die on the battlefield from a mysterious condition which was alleviated only late in the war by physiologist William Bayliss and others. Concerning this, in 1920 after hostilities ended, Bayliss came to the Ri to discourse on "The Volume of the Blood and its Significance".
Bayliss, of the same generation as Wright, was professor at University College London and advanced a field ripe for discoveries, although animal experiments won him notoriety. At the outbreak of war, he joined the Royal Army Medical College staff.
The volume of blood came especially into prominence in connection with the explanation and treatment of the state known as 'surgical shock', but which occurred with an alarming frequency in men wounded in the late war.
"Much difficulty was found in distinguishing between this state, even when attended by very little loss of blood, and that resulting from very great loss of blood unaccompanied by serious injury."
Bayliss’ experiments in 1916 pointed to the effective treatment eventually introduced, but it now seems that at that moment Bayliss was too reticent, and multitudes continued to die unnecessarily.
The capillaries dilated and leaked into surrounding tissue, dangerously lowering the blood pressure. It was suggested that the culprit was the body’s own production of histamine. It is now known that the causes are more complex.
"Blood has not actually been lost, and it should be possible to keep up an effective circulation by some other liquid until the poison is got rid of and the pooled blood returned to circulation. An innocuous fluid seemed to serve practically as well as blood, and had the advantage of being always at hand."
Just before the end of the war Bayliss and colleagues were able to avoid deaths from shock with another ‘dose of salts’, a simple mixture of saline solution, and gum which raised the osmotic pressure of the solution close to that of real blood.
About the author
Laurence Scales leads London tours featuring the history of science, invention and medicine. He is a graduate in engineering who has worked in various technological industries. He can be found on Twitter as @LWalksLondon